Abstract
Background: Multiple factors have contributed to the decline of classical hematology (CH) as a specialty. CH-workforce shortage coupled with overwhelming demands for CH consultations have created a crisis. This CH crisis may be especially acute at academic centers where CH is practiced in the milieu of cancer-care. This has broad effects on the quality of CH care, on the referral systems, and on the careers and professional satisfaction of hematologists at these centers focused on CH and on those focused on hematological malignancies. The objective of this study was to conduct an analysis of CH outpatient-referrals in order to develop strategic plans for dealing with the CH crisis.
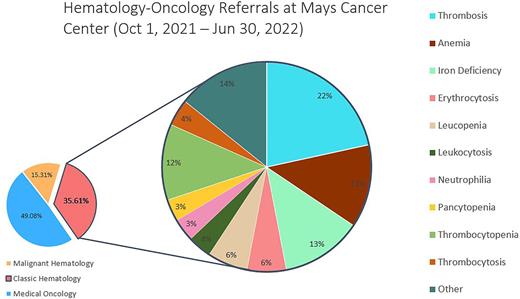
Methods: A single referral office at the Cancer Center (CC) handles all adult (age >18 years) hematology referrals (electronic and all other). All hematological malignancies are triaged immediately for ideal scheduling by specific Cancer-Center algorithms and are not part of this study. From October 1, 2021 to June 30, 2022, all other referrals to hematology were prospectively triaged daily by one of the authors (A.B.K) to define the category of CH problem from the reason for referral given by the referring provider. Referrals were not refused unless confirmed at triage that no CH problem was evident, and those turned away are included as part of this analysis. Video-based appointments were offered for all Thrombosis referrals and for confirmed iron deficiency anemia. Electronic consultation (opinion rendered without patient seen) at our CC is available exclusively for select CH problems and restricted to patients with Medicare who give written consent and are not part of this analysis.
Results: A total of 1505 CH referrals were received in the 9-month period. Of these, 951 (63%) were female, and 551 male (37%) with median age 53 (range 18-92 yrs.). 67 referrals (4.5%) were turned down. Of these, 25 were solid tumors, 21 were not hematology problems, 12 had normalized their abnormal hematology laboratory data (that were the basis of the referral), 8 with MGUS were triaged to the plasma cell-disorder clinic, and one 15-yr-old was referred to pediatric hematology. During the study-period, there were 2074 medical oncology referrals and 647 referrals for malignant hematology. CH referrals therefore comprise 36% of all hematology-oncology referrals and 70% of all hematology referrals at the Cancer Center. Thrombotic disorders were the most common of the accepted CH referrals at 311 (22%); of these 199 (64%) were for VTE. Other categories included 185 (13%) referrals for anemia, and 181 (12.7%) for iron deficiency. Video-visits were used for 294 of all CH referrals (20%), and the rest were in-person.
Conclusions: CH referrals are a little more than one third of all hematology and medical oncology referrals at the CC. Telemedicine (video) visits and elimination of barriers to electronic consultations for select CH problems can help cope with the demands for CH consultation. There are significant opportunities for partnership with and education for primary care services to care for straightforward CH referrals (iron deficiency and provoked venous thromboembolism) that will substantially reduce costs and enhance quality of care. Significant increase in faculty focused on CH is needed to cope with current demand, especially if CH services and special programs (Thrombosis Clinic, Hemoglobinopathy Clinic, and Rare Hematological Disorder Clinic) are to be advertised. This shift will also allow focused career-development for hematologists at the CC.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.